What is Pancreatitis?
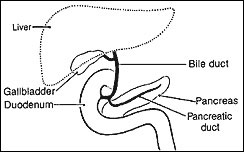
Pancreatitis is a disease in which the pancreas becomes inflamed. Pancreatic damage happens when the digestive enzymes are activated before they are released into the small intestine and begin attacking the pancreas according to wedmd.com. Under normal circumstances, your pancreas produces digestive enzymes that do not become active until they reach the small intestine. Once there, they help your body break down fats, proteins and carbohydrates as part of the digestive process. However, if these enzymes become active within the pancreas, they can cause acute or chronic bouts of inflammation.